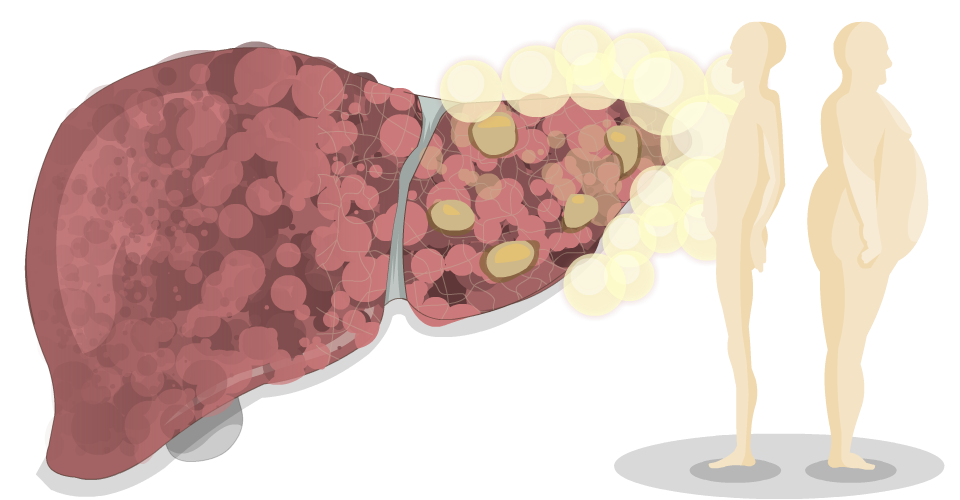
Fatty liver disease happens when fat builds up in the liver. This can cause the liver to become inflamed or enlarged, and over time, it may lead to liver damage.
The scientific name for fatty liver disease used to be non-alcoholic fatty liver disease (NAFLD). The updated name is metabolic dysfunction-associated steatotic liver disease (MASLD). You may still hear or see the old name (NAFLD), especially in older materials, but both terms refer to the same condition.
In some people, the fat in the liver causes inflammation and eventually scarring. This more severe form of the disease was previously called non-alcoholic steatohepatitis (NASH). It is now known as Metabolic dysfunction-associated steatohepatitis (MASH). This condition can progress to cirrhosis and liver cancer in some cases.
Causes
Fatty liver disease (MASLD) most often occurs in people with:
-
Type 2 diabetes
-
High blood pressure
-
Obesity
-
High cholesterol
These conditions often occur together and are known as metabolic syndrome. As our population becomes more sedentary and eats a less healthy diet, these risk factors—and fatty liver disease—are becoming more common.
Although it’s most often seen in people between the ages of 40 and 60 with one or more of these risk factors, fatty liver disease can also occur in people without any of them. It is now being diagnosed in children and young adults as well.
Symptoms
In the early stages of fatty liver disease, you may have no symptoms. Most people feel fine and don’t know they have it.
As the disease progresses and liver damage gets worse, you may have vague symptoms such as:
- an ache in the upper right part of your belly
- fatigue
- poor energy levels
Diagnosis
Fatty liver disease can be diagnosed with blood tests and radiology tests such as an ultrasound, CT scan, or MRI. A liver biopsy may also be needed. Talk to your healthcare provider if you’re overweight or if you have high blood sugar or cholesterol.
Treatment
There are a number of effective ways to treat fatty liver disease:
- Lose weight. Weight loss is a key aspect of treatment. Fatty liver disease can be reversed if you lose weight. Make a weight loss plan with your healthcare providers, and exercise to keep weight off.
- Exercise. Exercise means exerting yourself. You will know because you’ll feel breathless, and you’ll sweat. Start slowly if you’ve been inactive, for example brisk walks 5 to 10 minutes long. Build up to 30-minute brisk walks five days a week, adding in hills or stairs. Your healthcare providers can help guide you.
- Avoid alcohol. The current medical recommendation is that if you have fatty liver disease, you should avoid all alcohol. This is because alcohol also increases liver fat and may compound the problem.
- Get treatment for high blood sugar, hypertension, and elevated cholesterol. Medications can help to lower blood sugar, blood pressure, and cholesterol. In turn, this reduces fat in the liver. Ask your healthcare provider if you have these conditions and if medications are a good option for you.
You can have both fatty liver disease and another liver disease at the same time. Having two liver diseases can cause more liver damage and serious medical complications. If you have two liver diseases, it’s even more important to lose weight and exercise. By doing these things, you can treat both diseases at the same time.

References:
The information on this page was adapted (with permission) from the references below, by the Cirrhosis Care Alberta project team (physicians, nurse practitioners, registered nurses, registered dietitians, physiotherapists, pharmacists, and patient advisors).
This information is not intended to replace advice from your healthcare team. They know your medical situation best. Always follow your healthcare team’s advice.
References:
